USS TELESFORO TRINIDAD CAMPAIGN (USSTTC) “Ship and Shipmate Before Self”
MISSION: Name a US Navy Warship (Destroyer--DDG or Frigate--FFG) after Fireman Second Class Telesforo Trinidad, an American national of Filipino descent who received the Medal of Honor on April 1, 1915, for extraordinary heroism and intrepidity in the line of his profession to memorialize his heroic contributions to the U.S. Navy and our grateful Nation.
VISION: Perpetuate PO2 Trinidad’s heroic contributions to promote national awareness and education and bring pride and honor to the US Navy, its Sailors – officer and enlisted, their families and our Republic.
WHO WE ARE: USSTTC is a national grass roots advocacy group comprised of serving and retired members of the US Armed Forces, community leaders, academics, corporate executives, civic leaders, partners and sponsors, and veterans’ families committed to naming a US Navy Warship after Trinidad. (A 501(c)(3) application is in progress).
BACKGROUND: No US Navy ship has been named after a member of the US Armed Forces of Filipino descent, even though tens of thousands of Filipinos have served faithfully in the US Navy beginning in 1901 when President William McKinley signed an Executive Order allowing the Navy to enlist 500 Filipinos as part of the Insular Force. Approximately 6,000 Filipinos enlisted in the US Navy during WWI and many more joined through the interwar period leading up to WWII. After the Philippines obtained its independence from the United States in 1946, over 35,000 Filipinos were recruited into the US Navy from 1952 to 1992 under a provision of the Republic of the Philippines- United States Military Bases Agreement. In addition, thousands of Americans of Filipino descent enlisted during this same 40-year period, and continue to do so until today.
DISCUSSION: Trinidad remains the first and only American of Asian descent and first American national of Filipino descent in the US Navy to receive a Medal of Honor for his extraordinary heroism in the line of his profession during boiler explosions onboard the USS San Diego (ACR-6) while the ship was underway in the Gulf of California on January 21, 1915. Trinidad brought two crewmembers to safety in spite of his own physical injuries from the explosion. He was awarded the Medal of Honor in accordance with General Order Number 142 signed by the Secretary of the Navy Josephus Daniels on April 1, 1915.
To date, there is only one ship, the USS Chung-Hoon (DDG-93) named after an Asian American in the Navy - Rear Admiral Gordon Pai’ea Chung-Hoon, Commanding Officer of USS Sigsbee (DD-502) during World War II, who received the Navy Cross for his gallant actions during a kamikaze attack on April 14, 1945.
RECOMMENDATION: Name a US Navy Warship-- Destroyer or Frigate--after PO2 Telesforo Trinidad, which follows in the proud tradition of the US Navy in naming a ship after a Medal of Honor Recipient.
POINT OF CONTACT: Cecilia I. Gaerlan
Email: cecilia@bataanlegacy.org; Cell: (510) 520-8540
The Moral Determinants of Health: Purpose, Promise, and Propositions - Part 2 The Promise for the Betterment of Health
Nelson Tuazon, DNP, DBA, RN, NEA-BC, CENP, CPHQ, CPPS, CPXP, FNAP, FACHE, FAAN
Vice President & Associate Chief Nursing Officer, University Health
Director, District 8, Texas Organization for Nursing Leadership
In Part One of this article on The moral determinants of health: Purpose, promise, and propositions (Tuazon, 2021), the focus of the discussion was on aligning the work of healthcare professionals and providers with purpose. I presented the background and traced the development of the moral determinants of health. I focused on moral theories as a framework for determining the purpose of the moral determinants of health. In this Part Two, I will explore the promise of the moral determinants of health in conjunction with the social determinants of health. Specifically, I will explore whether the moral determinants of health intersect with the social determinants of health or if they are considered an evolution.
Health Gap: Creating the Social Movement
As I have stated in Part One, I came up with more questions, rather than specific answers to the question of "What's new about the moral determinants of health." The complexity surrounding moral issues leads to more questions. Similar to the experience of the World Health Organization’s (WHO) Commission on the Social Determinants of Health (CSDH), there is a need for more research to gain an understanding of the moral determinants of health. However, in his commentary on the social determinants and the health gap, Marmot (2017) emphasizes the need for action amidst the pressing normative and empirical questions on the social determinants of health. I submit that we can take the same approach as we examine and explore the promise of the moral determinants of health. Similar to the social movement that Marmot (2017) has advanced, social responsibility is critical to addressing the health gap and the social and moral determinants of health. With regards to health and healthcare, social justice can be applied at the individual, community, national or regional, and international levels (Bhugra, 2017).
The Moral Determinants of Health: Shared Endeavor
The primary premise of the moral determinants of health is based on the assumption that “the moral law within commands shared endeavor for securing the health of communities” (Berwick, 2020, p. 225). As the harbingers and champions of the promise for the betterment of health, physicians, nurses, other healthcare professionals, and healthcare institutions must advocate for and lead a series of actions. The list could be long but the immediate priorities encompass the following (Berwick, 2020; Commins, 2019):
Ratifying the basic human rights treaties and conventions of the international community by the U.S.,
Recognizing healthcare as a human right in the U.S.,
Restoring U.S. leadership on climate change,
Reforming the criminal justice radically,
Implementing immigration reform,
Ending hunger and homelessness, and
Restoring order, dignity, and equity to U.S. democratic institutions and ensuring that every legal vote is counted.
Claiming the Moral Determinants of Health into the Healthcare Lane
This initial list that comprises the moral determinants of health, albeit short, is daunting and overwhelming. Berwick (2020) opines that some may say that the agenda for the moral determinants of health is outside the realm of traditional healthcare – that is, to care for those who are ill. However, the long-standing issues of inequities and disparities in our healthcare delivery system should compel healthcare professionals to act on these moral determinants of health. In 2005, the WHO established the CSDH to turn public-health knowledge into political action (Marmot, 2005). While the focus of this Commission is neither new nor surprising, poverty remains a critical and complex issue when it comes to inequalities in healthcare. The time has come that the moral determinants of health that impact the health of vulnerable populations fall within the healthcare lane (Berwick, 2020).
The Promise for the Betterment of Health: The Moral Determinants of Health
Any discussion on the relationship between healthcare and efforts to improve social conditions, counteract inequity and disparities, and fight against structural racism evokes emotional, mental, and psychological responses. Because of their political nature, there is disagreement on these issues even among honest and compassionate people. The traditional belief that healthcare should be confined to treating and caring for illness is still espoused by some (Berwick, 2020). Exploring the promise of the moral determinants of health merits our attention. Below is a brief exploration on the promise of the moral determinants of health.
Basic Human Rights Treaties and Conventions. The U.S. was a leader in shaping the United States Charter and the Universal Declaration of Human Rights (UDHR) (Simcox, 2018). The UDHR has become the “basis for health and human rights thinking, advocacy, scholarship, and actions” (Beyrer, 2020, p. 359). However, the U.S. has not fully ratified or advanced all of the nine core human rights conventions that have been adopted by the UN General Assembly. These unratified conventions involve economic, social, and cultural rights; all forms of discrimination against women, the rights of the child, the migrant workers, and their families, and persons with disabilities (Berwick, 2020). Three U.S. administrations have viewed economic, social, and cultural rights as desirable social goals, rather than rights. Additionally, only three of the treaties have been ratified including the 1966 UN Convention on Civil and Political Rights, the 1966 Convention on the Elimination of Racial Discrimination, and the Convention against Torture. Since the founding of the UN International Labor Organization (ILO), the U.S. has ratified only 14 of the 189 ILO conventions (Simcox, 2018).
Healthcare as a Human Right. Khosla (2020) chronicles three significant events that marked the serious attention that has been given to human rights in health at the global level. These include the establishment of the Francois-Xavier Bagnoud Centre on Health and Human Rights at the Harvard School of Public Health in 1993; the call for the universality, indivisibility, and interdependence of all human rights during the World Conference on Human Rights held in Vienna in 1993; and the appointment of the first UN Special Rapporteur on Right to Health in 2020 (Khosla, 2020, p. 335). Berwick (2020) laments that the staggering number of uninsured individuals – approximately 30 million – compels us to push for the recognition of healthcare as a human right.
Climate Change. The effects of climate change on health systems include a) costs, which are estimated to be in the order of trillions of dollars; b) utilization of healthcare services depending on climate change exposure; c) disruption of care caused by extreme weather; and d) undermining of public health infrastructure and global health achievements (Salas & Solomon, 2019). The recent winter storm in Texas significantly affected healthcare delivery due to the disruptions in electricity, water supply, food distribution, equipment and supplies, transportation, and other essential services and resources in the community. Ryan et al. (2018) have explored the application of systems thinking for health promotion and climate change adaptation. Their preliminary evidence demonstrates the benefits of joined-up action on climate and health, exploring the negative health impacts of climate change, particularly in rural areas (Ryan et al., 2018, p. 569). The recent developments have indicated that the U.S. is taking a leadership role in addressing climate change. Both proponents and skeptics to the greater involvement of the U.S. in leading the climate change agenda have expressed their concerns. I submit that healthcare providers and nurses will remain steadfast in addressing the impact of climate change on health and healthcare. Belkin (2020) posits that social and emotional resilience will determine our ability to adapt to or mitigate, endure, and enact policies related to climate and ecologic change.
Criminal Justice Reform. Miah (2020) provides compelling arguments for the abolishment and replacement of the U.S. criminal legal system. He posits that the U.S. has two de facto criminal legal systems – one for African Americans and people of color and the other for whites (Miah, 2020, p. 4). Rappaport (2020) provides an equally compelling description of the ills of the U.S. criminal justice system including unprecedented levels of incarceration, disproportionate numbers of incarceration across racial groups, and police that hurt people whom they have a duty to serve and protect. He warns though that the democratization of the criminal justice system, although appealing, will not truly fix what ails us (Rappaport, 2020, p. 711). With regards to health and healthcare delivery, Harzke and Pruitt (2018) provided a comprehensive summary of the prevalence of medical conditions in U.S. prisons and jails. They examined the determinants and progression of these medical conditions and made recommendations to improve a) measurement of the burden of chronic medical conditions, b) healthcare delivery in correctional settings; and c) continuity of care post-release and re-entry into the community.
Immigration Reform. The topic of immigration continues to be a controversial U.S. public policy issue. Any discussion on immigration will likely involve issues on the burdens that immigration places on the U.S. population, public assistance, health, and educational systems. Regardless of one's position on the immigration debate, the issues center around the protection of the interests of U.S. citizens on the one hand, and the addition of new labor and innovative thinking that benefit the U.S. economy and all Americans, on the other hand (Bean, 2020). Immigration policies should be more incremental, specific, and pragmatic. They should be visibly and directly connected to economic benefits to the middle class (Peri, 2020).
Ending Hunger and Homelessness. Hunger in America, one of the richest countries in the world, persists. It has been projected that more than 50 million Americans faced hunger in 2020, exacerbated by COVID-19. This was up from 35 million before the pandemic. This means that 1 in 6 individuals, including 1 in 4 children suffered from hunger (Villareal, 2020). The National Healthcare for the Homeless Council (2019) provides alarming statistics on homelessness in the U.S. It has been estimated that 1.5 million people experience homelessness annually; some believe that these numbers may be doubled. Individuals who are homeless experience higher rates of illness and have a shorter lifespan of 12 years compared to the general U.S. population. Unfortunately, as a part of a vicious cycle, poor health is a major cause of homelessness. The solution to this problem may seem obvious but is complex – stable housing. The Center for Disease Control and Prevention (CDC, 2020) provides resources on homelessness as a public health issue. Hunger and homeless are completely addressable issues (Berwick, 2020, p. 225).
Election Reforms. Not unlike the first six issues that have been presented, any discussion on election reforms evokes powerful sentiments and provokes heated debates. Berwick (2020, p. 226) posits that restoring order, dignity, and equity to U.S. democratic institutions is critical and ensuring the right of every individual’s vote to count equally is crucial. The American Organization for Nursing Leadership (2021) advocates for empowering nurses to vote and for the voices of nurses to be heard in local, state, and federal elections.
What Lies Ahead
The promise of the moral determinants of health may not be in sight soon enough. Due to the nature of the moral determinants of health and the present environment in which we live, “there is a visible decline in the willingness to take on issues that are now viewed to be too controversial or even radical” (Gruskin, 2020). We can only heed the advice from the WHO Review of the social determinants and the health divide: Do something, do more, do better! (Marmot, 2014). Is the impetus for advocating for moral justice to eliminate the health gap resonating to all of the healing professions? While the empirical evidence for the moral determinants of health is developing, we must take action at the individual and structural levels. Gruskin (2020) reminds us to be strategic and not just reactive to be able to address the crisis of the moment. For nurses, Maykut (2020) asserts that moral habitability – defined as the “intersect between the socio-political location of nurses and the ideologies and structure of workplace environments” – is necessary to ensure humanistic caring (p. 491). As healthcare administrators, nurse executives, and leaders, it is our responsibility to promote work climates that foster moral habitability among nurses at all levels.
Note: In the upcoming final section, Part Three, I will outline the propositions on the moral determinants of health with a focus on the role of nursing leaders.
References
American Organization for Nursing Leadership (AONL). (2021). Empowering nurses leaders to vote. Empowering Nurse Leaders to Vote | AONL
Bean, F. D. (2020). Why the United States must renew opportunities to achieve the American dream in order to reform immigration policy. Journal of Policy Analysis & Management, 39(1), 274–279. https://doi.org/10.1002/pam.22186
Belkin, G. (2020). Leadership for the social climate. The New England Journal of Medicine, 382(21), 1975-1977. doi:http://dx.doi.org.vlib.excelsior.edu/10.1056/NEJMp2001507
Berwick, D. M. (2020). The moral determinants of health. JAMA, 324(3), 225–226. https://doi.org/10.1001/jama.2020.11129
Beyrer, C. (2020). Impunity : Undermining the health and human rights consensus. Health and Human Rights, 22(1), 359–362.
Bhugra, D. (2017). Commentary: Social determinants, social discrimination, social justice, and social responsibility. International Journal of Epidemiology, 46(4), 1333-1335.
Center for Disease Control and Prevention (CDC). (2020). Homelessness as a public health law issue: Selected resources. CDC - Homelessness as a Public Health Law Issue - Publications by Topic - Public Health Law
Commins, J. (December 12, 2019). Berwick outlines sweeping 7-step campaign for quality movement. HealthLeaders, Retrieved from https://www.healthleadersmedia.com/innovation/berwick-outlines-sweeping-7-step-campaign-quality-movement
Gruskin, S. (2020). Reflections on 25 years of health and human rights : History, context, and the need for strategic action. Health and Human Rights, 22(1), 327–330.
Harzke, A. J., & Pruitt, S. L. (2018). Chronic medical conditions in criminal justice involved populations. Journal of Health & Human Services Administration, 41(3), 306–347.
Khosla, R. (2020). Health and human rights at a crossroads. Health and Human Rights, 22(1), 335–338.
Marmot, M. (2005). Social determinants of health inequalities. Lancet, 365, 1099-1104.
Marmot, M. (2014). Review of social determinants and the health divide in the WHO European Region: Executive summary. Review of social determinants and the health divide in the WHO European Region: Executive Summary
Marmot, M. (2017). Commentary: Social determinants and the health gap: Creating a social movement. International Journal of Epidemiology, 46(4) 1335-1339.
Maykut, C. A. (2020). Skillful moral leadership: Collective action to foster moral habitability. Nurse Leader, 18(5), 491–496. https://doi.org/10.1016/j.mnl.2019.09.020
Miah, M. (2020). Abolish and replace: The U.S. criminal legal system. Against the Current, 35(5), 3–4.
National Health Care for the Homeless Council (NHCHC). (2019, February). Homelessness & health: What’s the connection? homelessness-and-health.pdf (nhchc.org)
Peri, G. (2020). Can we get U.S. citizens to support immigration reforms? Journal of Policy Analysis & Management, 39(1), 279–281. https://doi.org/10.1002/pam.22187
Rappaport, J. (2020). Some doubts about “democratizing” criminal justice. University of Chicago Law Review, 87(3), 711–813.
Ryan, I., Patrick, R., Capetola, T., & Brown, J. (2019). Applying systems thinking to the climate‐health challenge. Australian Journal of Rural Health, 27(6), 568–570. https://doi.org/10.1111/ajr.12561
Salas, R. N., & Solomon, C. G. (2019). The climate crisis - health and care delivery. The New England Journal of Medicine, 381(8), e13. https://doi.org/10.1056/NEJMp1906035
Simcox, D. (2018, January 3). Where does the US stand on UN human rights conventions. Where does the US stand on UN human rights conventions? (cincinnati.com)
Tuazon, N. (2021, January). The moral determinants of health: Purpose, promise, and propositions. Part One: Aligning work with purpose. TONL Monthly. The Moral Determinants of Health: Purpose, Promise, and Propositions (naylornetwork.com)
Villareal, M. (2020, November 24). More than 50 million Americans facing hunger in 2020, projections show. More than 50 million Americans facing hunger in 2020, projections show - CBS News
The Moral Determinants of Health: Purpose, Promise, and Propositions
Nelson Tuazon, DNP, DBA, RN, NEA-BC, CENP, CPHQ, CPPS, CPXP, FNAP, FACHE, FAAN
Vice President & Associate Chief Nursing Officer, University Health
Director, District 8, Texas Organization for Nursing Leadership
Laying the Foundation
In his groundbreaking keynote speech during the 2019 Institute for Healthcare Improvement (IHI, 2020) National Forum titled, Quality, Mercy, and the Moral Determinants of Health, Dr. Donald Berwick paid homage to two leading quality experts in quality – Avedis Donabedian and W. Deming. In paying tribute to their pioneering work, Dr. Berwick ascribed the following quotes to them: "Ultimately, the secret sauce of quality is love," and "All anyone asks for is a chance to work with pride," respectively. He concluded his remarks with a poignant revelation about his insights on quality. Profoundly, he provoked us by asserting that quality should transform from its technical essence to the essence of morality. This was the seminal thesis that brought the concept of the moral determinants of health to the forefront.
Scope, Scale, and Substance
There is paucity in the literature with regards to the concept of moral determinants of health. As nurses, the third provision of the Guide to the Code of Ethics for Nurses stipulates that the "ultimate moral duties of professional nurses involve working with people who need nursing care" (Fowler, 2010, p. 25). I have to admit that in researching this topic, I came up with more questions than answers. I initially had predictions in the working title, but I opted to explore propositions to provoke the conversation that Dr. Berwick has sparked. In this three-part series, I will examine the purpose, the promise, and the propositions on the moral determinants of health. In Part One, I will review the background and trace the development of the moral determinants of health. I will be focusing on moral theories as a framework for determining the purpose of the moral determinants of health. In Part Two, I will explore the promise of the moral determinants of health in conjunction with the social determinants of health. Specifically, I will explore whether the moral determinants of health intersect with the social determinants of health or if they are considered an evolution, Finally, in Part Three, I will outline the propositions on the moral determinants of health with a focus on the role of nursing leaders.
The Ubiquity of Moral Issues
Regardless of our role in our healthcare facility or institution, or our professional organization, moral issues constantly barrage us (Kreitler et al., 2014). The issues come from different people at different times, with varying degrees of complexity. Our day may begin with the first call about staffing needs in the early hours of the morning and end with a late call-in at night. The 20 or so patients waiting in the emergency department and the backlog in the operating room continue to preoccupy us. The looming budget cuts because of the operational losses brought about by the pandemic bring anxiety. The competing demands to improve the scores on patient experience amidst the distress that the staff faces consume our energy. Likewise, the academic environment is not spared from these moral issues. De Barros et al. (2019) have identified various causes of moral distress among nursing faculty including changes and disruptions in work processes, increased workload, competing priorities, lack of time, resources, and support, among others. Grace (2018) stated that nurse leaders and educators are ill-prepared to help in the development of the moral agency of nurses due to the lack of ethics education in academia. Students are also subjected to ethical conflicts and dilemmas that can affect their working potential and may cause physical and mental health issues. Moral distress among nursing students is a reality (Renno et al., 2018).
Physicians are not isolated from the moral issues surrounding healthcare. The competition for the allocation of resources – driven greatly by increases in new technologies and new drugs – puts the physicians in moral dilemmas. The promise of advances in technologies and pharmaceuticals is tempered by the high costs. This also comes with the recognition that the demands for healthcare care may be infinite but the resources are finite (Mallia, 2020).
Purpose of MDOH
In his book, Man's Search for Meaning, Victor Frankl (1959), asserts that humans seek meaning by committing to a cause or purpose outside of themselves. To understand the purpose of the moral determinants of health, it is important to distinguish and ascertain what constitutes or contributes to the notion of what is "right" in healthcare (Commins, 2019). Berwick submits that the following determine and influence the betterment of health (Berwick, 2020)
Ratifying the basic human rights treaties and conventions of the international community by the U.S.,
Recognizing healthcare as a human right in the U.S.,
Restoring U.S. leadership on climate change,
Reforming the criminal justice radically,
Implementing immigration reform,
Ending hunger and homelessness, and
Restoring order, dignity, and equity to U.S. democratic institutions and ensuring that every legal vote is counted.
Framework for Ethical Decision-Making
The theoretical frameworks for analyzing the moral determinants of health may fall under teleological or deontological theories. Teleological theories are concerned with ends, goals, purposes, or consequences. Deontological theories, on the other hand, are concerned with duty, doing what is right because it is right. Generally, tools that are used to evaluate moral and ethical decision-making include five broad stages (Kreitler et al., 2014). These include a) defining the situation, b) generating alternatives, c) evaluating the alternatives, d) selection, and e) action.
Moral Theories: Understanding Moral Issues
The complexity of moral issues requires that the analysis of these issues begins with facts. The assertion that health is determined by moral factors necessitates an understanding of the ways that we evaluate moral issues. The five general approaches to appraise moral issues include the a) utilitarian approach, b) rights approach, c) fairness or justice approach, d) common-good approach, and e) virtue approach (Velasquez et al., 2014). When evaluating issues based on which actions provide the greatest balance of good over evil, the utilitarian approach is in use. Although the approach seems straightforward, the determination requires a series of steps. The first is to identify different available actions. This is followed by the question of who will be affected by each action, either causing benefits or harm. Finally, the action that produces the greatest benefits and the least adverse outcomes for the greatest number of affected individuals is selected. The rights approach presupposes that individuals can freely choose their actions affecting their lives and that this choice should be respected. The fairness or justice approach requires the treatment of everyone fairly, without favoritism or discrimination. The common-good approach assumes that an individual's good is inseparably tied to the good of the community and society. Finally, the virtue approach requires recognition of certain ideals for which every individual should strive, which will result in the full development of humanity (Velasquez et al., 2014).
In attempting to resolve ethical issues in healthcare, it is noteworthy to heed the advice and warning given by Upton (2011). He avers that there is currently a "lack of any generally accepted method of solving moral problems, together with the extreme improbability of philosophy achieving a plausible determinate theory" (Upton, 2011, p. 431). Because of this reason, we are directed to be open to theorizing rather than using moral theories in our attempts to solve moral issues in healthcare. On the other hand, Miller (2016) commends the efforts and contributions of authors and editors in demonstrating the critical role of theory and philosophy in the ongoing healthcare reforms, particularly with regard to national healthcare policy (p. 128).
Benchmarks for the Fairness Test
The issue of fairness or justice is at the core of the moral determinants of health. A focal point of debate and discussion is whether healthcare is a right (Commins, 2019, IHI, 2020). Amidst the massive healthcare reforms, the issue of fairness is either concealed or disregarded. The two primary reasons for the weak or absent deliberations on fairness are the difficulty in defining fairness and lack of the essential concepts and vocabulary within mainstream economics (Caplan et al., 1999). In essence, neoclassical economics "has neither the necessary moral vocabulary nor a hierarchy of moral value (Caplan et al., 1999, p. 855). In other words, moral theories may not be the sole and ultimate basis for addressing moral determinants of health.
Is the U.S. Healthcare System Fair?
The answer to this question is not easy because of the inherent complexity of the U.S. healthcare system. Caplan et al. (1999, p. 858) offered ten benchmarks upon which the fairness of the reforms in the U.S. healthcare system can be evaluated. These include:
Universal access – coverage and participation,
Universal access – minimizing nonfinancial barriers,
Comprehensive and uniform benefits,
Equitable financing – community-rated contributions,
Equitable financing – the ability to pay,
Value for money – clinical efficacy,
Value for money – systemic efficiency,
Public accountability,
Comparability, and
Degree of consumer choice.
The readers are encouraged to read more about these benchmarks in detail to understand how these benchmarks can be applied. The authors offered a numerical system of scoring to assess for fairness. Although public input is promoted and encouraged when healthcare reforms are made in the U.S., public debate is uneven and discriminatory (Caplan et al., 1999, p. 866).
Role of Nurses
Amidst the considerable reforms in the U.S. healthcare system that are taking place – and more is necessary and essential – nurses will continue to play a vital role in addressing the persistence of healthcare disparities and the rapidly increasing healthcare costs. Nurses at all levels have the moral imperative to help shape health and social policies (Mason, 2016). Nurses are also caught between economic priorities and their ability to ensure the delivery of equitable care to their clients. Nurse leaders must continue to take part in the decision-making process and to have their voices heard with regard to health policies that foster quality. Ultimately, they must forge and sustain an environment for moral agency (Maykut, 2020, p. 491).
In my own pragmatic way, here are my thoughts on Dr. Berwick's shortlist of agenda for action on the moral determinants of health. As I have mentioned, I had more questions than answers when I was researching this topic. My questions are by no means exhaustive.
As nurse executives, administrators, and practice leaders:
Do we have an institutional mission/vision/value statement, and do we operate according to those values?
What are our policies and procedures in ensuring that the rights of our patients are enforced?
How do we ensure that the rights of homeless, non-citizens or those from jail that come to our ER and hospitals receive the care they need?
How do we assess food insecurity, among others, as part of our discharge planning?
How have we collaborated with community leaders to address the needs of the homeless?
As faculty, academicians, and researchers:
How do we educate our students on the moral determinants of health?
How have we integrated ethical decision-making into our curriculum?
Have we encouraged students, especially doctoral students, to consider these topics as part of their capstone or dissertation?
Have we published or written an op-ed on any of the moral determinants of health?
As leaders and members of our professional associations:
How have we incorporated these moral determinants of health in our mission and vision statements?
What programs, activities, or initiatives have we taken to address climate change, hunger, and homelessness, or any of the 17 Sustainable Development Goals by the United Nations (UN, n.d.)?
How have we advocated for healthcare as a human right or immigration reform?
How have we promoted that each of our members exercises their right to participate in elections and vote?
Parting Words
As I mentioned earlier in this paper, I had more questions than answers as I was preparing for this article. The concept of the moral determinants of health is relatively new and there has not been a lot of information that has been published on this topic. I would like to open the dialog and pose the following questions. Please send me your thoughts to Nelson.Tuazon@uhs-sa.com. With your permission, I would like to include your ideas in Parts Two and Three of this article in the next couple of issues of TONL Monthly.
What are your thoughts on the moral determinants of health?
Are there other moral issues that you would like to see added to Dr. Berwick's list?
What is the role of nursing – practice, academia, research, and nursing leadership – with regards to the moral determinants of health?
Author's Notes:
Part Two: The Social and Moral Determinants of Health: Intersection or Evolution?
The next part of this article will explore whether the moral determinants of health intersect with the social determinants of health or if they are an evolution of the social determinants of health. The focus of the discussion will be on the promise of the moral determinants of health.
References
Berwick, D. M. (2020). The moral determinants of health. JAMA, 324(3), 225–226. https://doi.org/10.1001/jama.2020.11129
Caplan, R. L., Light, D. W., & Daniels, N. (1999). Benchmarks of fairness: A moral framework for assessing equity. International Journal of Health Sciences, 29(4), 853-869.
Commins, J. (December 12, 2019). Berwick outlines sweeping 7-step campaign for quality movement. HealthLeaders, Retrieved from https://www.healthleadersmedia.com/innovation/berwick-outlines-sweeping-7-step-campaign-quality-movement
de Barros, A. M., Ramos, F. R. S., Barth, P. O., Brito, M. J. M., Rennó, H. M. S., & Rocha, J. M. (2019). The moral deliberation process of college nursing professors in view of moral distress. Nurse Education Today, 73, 71–76. https://doi.org/10.1016/j.nedt.2018.11.014
Frankl, V. (1959). Man's search of meaning. Beacon Press.
Grace, P. (2018). Enhancing nurse moral agency: The leadership promise of Doctor of Nursing Practice preparation. Online Journal of Issues in Nursing, 23(1), 1. https://doi.org/10.3912/OJIN.Vol23No01Man04
Institute for Healthcare Improvement (IHI). (2020, January 7). Quality, mercy, and the moral determinants of health. YouTube. [Video). 2019 - Quality, Mercy, and the Moral Determinants of Health - YouTube
Kreitler, C. M., Stenmark, C. K., Rodarte, A. M., & DuMond, R. P. (2014). ACED IT: A tool for improved ethical and moral decision making. Journal of Moral Education, 43(4), 447-467.
Mallia, P. (2020). Allocation of resources in medicine – a moral imperative for doctors as well. Medicine, 48(10), 671–674. https://doi.org/10.1016/j.mpmed.2020.07.002
Mason, D. J. (2016). Promoting the health of families and communities: A moral imperative. Hastings Center Report, 46, S48–S51. https://doi.org/10.1002/hast.633
Maykut, C. A. (2020). Skillful moral leadership: Collective action to foster moral habitability. Nurse Leader, 18(5), 491–496. https://doi.org/10.1016/j.mnl.2019.09.020
Miller, R. B. (2016). Healthcare as a moral practice. Journal of Theoretical and Philosophical Psychology, 36(2), 128–130. https://doi.org/10.1037/teo0000042
Rennó, H. M., Ramos, F. R., & Brito, M. J. (2018). Moral distress of nursing undergraduates: Myth or reality? Nursing Ethics, 25(3), 304.
United Nations. (n.d.) Sustainable development goals. Retrieved from THE 17 GOALS | Sustainable Development (un.org)
Upton, H. (2011). Moral theory and theorizing in health care ethics. Ethical Theory & Moral Practice, 14(4), 431–443. https://doi.org/10.1007/s10677-011-9295-6
Velasquez, M., Andre, C., Shanks, T., & Meyer, T. (2014). Thinking ethically: A framework for moral decision-making. Retrieved from Thinking Ethically (scu.edu)
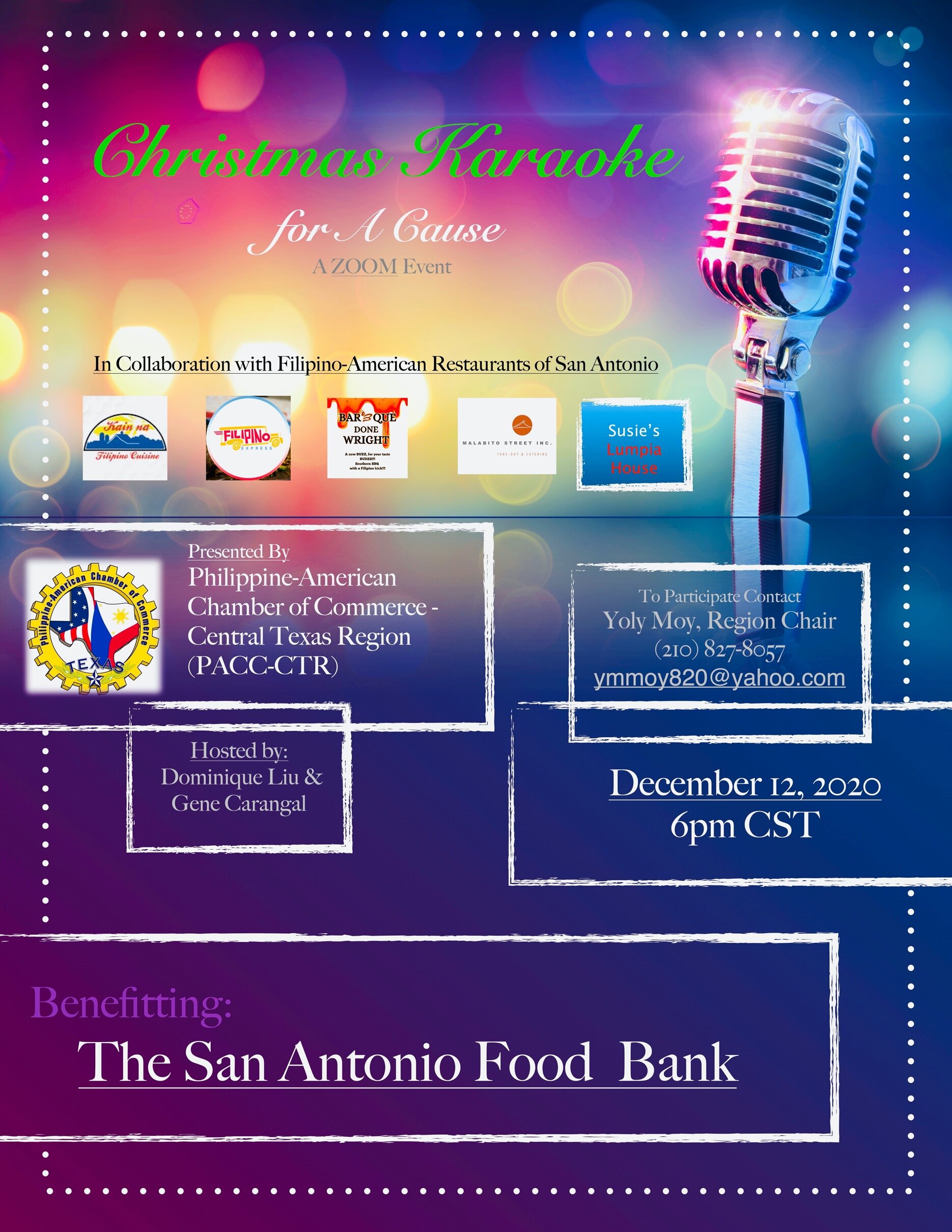
Christmas Karaoke for A Cause Video
The 2020 Christmas Karaoke for A Cause Zoom event is now available on YouTube. Please visit our GoFundMe page at https://gf.me/u/zbxguq to contribute to the our fundraiser for the San Antonio Food Bank.
San Antonio Food Bank Fundraiser
On behalf of the Philippine-American Chamber of Commerce, Central Texas Region, we would like to announce our Christmas Karaoke Event to benefit the San Antonio Food Bank. You can contribute to this great cause by going to https://gf.me/u/zbxguq
We are collaborating with San Antonio’s Filipino-American Restaurants to help raise funds for families in need of meals this holiday season.
~
Make your holiday cooking Hassle-Free and order from our participating Filipino-American Restaurant Partners:
Kain Na - Filipino Cuisine
Filipino Express
Bar B Que Done Wright
Susie's Lumpia House
Malabito Street Take-out & Catering
Self-Leadership: Leaders’ Intentionality, Influence, and Impact
Nelson Tuazon, DNP, DBA, RN, NEA-BC, CENP, CPHQ, CPPS, CPXP, FNAP, FACHE, FAAN
Vice President and Associate Chief Nursing Officer, University Health
Director, District 8, Texas Organization for Nursing Leadership
When one observes the language that we use in response to the current societal influences and the environment in which we live, the tone and tenor signal a sense of urgency and anxiety. Words and phrases such as the new norm, surge, twindemic, infodemic, psychological safety, emotional PPE (personal protective equipment), resiliency, recovery, and the like, evoke various emotional, psychological, and intellectual responses. More than ever, nurse leaders must be open to new ways of coping, new approaches to learning, and new imperatives for leading (Fuchs, 2020; Lacey, 2020; Tuazon, 2020).
Information Overload in Times of VUCA
As leaders, we face an information war where we live, where we play, and where we work. The current pandemic has led to the constant pouring of data and deluge of information that could paralyze us in our decision-making. Information overload has been known to be associated with stress and can affect analytical and intuitive thinking and critical thinking disposition (Misra et al., 2020). Information comes fast and furious and on different platforms including traditional and digital media (Ahmed, 2020). Regardless of the position or title we hold and irrespective of the scope of our work, or role in a professional organization, we plunge and rummage through bits and bytes to direct our problem-solving and decision-making. The paperwork piles up – quality and safety reports, patient experience scores, financial accounts, and committee and task force meeting minutes, to name a few. The deadlines and timelines put additional pressure on the already hectic schedules of nursing leaders. This phenomenon could be equated to the VUCA (volatility, uncertainty, complexity, ambiguity) world, a phenomenon with roots from the leadership theories of Bennis and Nanus (1985).
How to Manage in the VUCA World
The world of nurse leaders is characterized by increasing complexity and demands of time, energy, and resources, which often cause stress, fatigue, and burnout (Remegio et al., 2020). During times of crisis such as the COVID-19, gaps in leadership are magnified and intensified. The three factors that have impacted the current crisis include disruptions in operations that shifted organizational strategies, accelerated use of digital information and technology, and managing a workforce that may have been dispersed and work remotely (Study: COVID creates leadership gap, 2020). Engagement among leaders is crucial and essential to affect organizational change and foster organizational culture (Bywater & Lewis, 2019; Remegio et al., 2020).
Johansen (2012) adapted the original VUCA and offered the following to combat the chaos associated with this phenomenon: Vision, Understanding, Clarity, and Agility. With the shift from the pervasive negative aspects of VUCA caused by the pandemic, leaders must lead with new and renewed perspectives. Lacey et al. (2020) advise leaders to acknowledge the reality of needing to endure this crisis. They urge leaders to decide with speed and be comfortable with the gray zone on imprecision. Effective leaders adapt with boldness and admit limitations and lack of knowledge of some things with humility. With the information and knowledge that is known at the moment, leaders deliver outcomes and results reliably. Bywater and Lewis (2019) challenge us to examine the competencies required to lead in a VUCA world. They acknowledge that leadership agilities, including context-setting agility, stakeholder agility, creative agility, and self-leadership agility, are critical competencies but require further examination, especially in times of high change such as the pandemic. Amidst the many challenges and adverse conditions that we face currently, visionary leaders have the convictions that these can lead to the rebirth of their organizations (Lacey et al., 2020).
Self-leadership Agility
The concepts behind self-leadership are not new. In the past four decades, scholars have examined the construct of self-leadership particularly because of its capacity to affect and influence personal effectiveness (Crisostomo & Giardino, 2020). Self-leadership is defined as a process that encompasses three major concepts, including self-knowledge, self-influence, and self-guidance (Ay et al., 2015). There are three generally accepted approaches to self-leadership. These include constructive thought strategies, behavior focused strategies, and natural reward strategies (Bryant & Kazan, 2012) (See table 1). The scope and scale of self-leadership encompass two paradigms – self-leadership in general and self-leadership within organizations (Manz, 2015). There is a plethora of evidence that demonstrates the benefits of self-leadership to the individual and the organization (Abid et al., 2020; Furtner et al., 2018; van Dorssen-Boog et al., 2020). To the individual, self-leadership is associated with heightened self-awareness, greater mindfulness, and enhanced self-confidence. On a personal level, self-leadership results in realizing meaning and purpose improved interpersonal relationships and increased happiness. To the organization, effective self-leadership yields increased engagement and empowerment, improved decision-making, improved work performance, and enhanced creativity and innovation (Abid et al., 2020; Ay et al., 2017; Bryant & Kazan, 2012; Kim & Sim, 2020; Sahi, 2017; Stewart et al., 2019).
Table 1. Self-Leadership Strategies, Characteristics, and Outcomes
| Self-Leadership Strategies | Characteristics | Outcomes |
|---|---|---|
| Constructive Thought Strategies |
|
Job autonomy, work engagement, and mindfulness. |
| Behavior Focused Strategies |
|
Achievement and completion of difficult, tedious, or challenging tasks. |
| Neutral Rewards Strategies |
|
Shifting of focus from unpleasant to positive and more rewarding experiences. |
Intentionality, Influence, and Impact
Intentions, influence, and impact intersect within the context of self-leadership. Intentions differ from intentionality. Whereas intentions pertain to the course of action that the individual takes, intentionality denotes consciousness of actions and the awareness of many potential perspectives and goes beyond one’s understanding of experience. The degree of consciousness not only involves rational thinking and critical reflection but also involves social awareness of others (McDonald, 2019). In other words, intentionality is more than having mere intentions. Influence pertains to the result of purposeful action. Self-leaders must have a positive influence on themselves and the world around them to enable them to affect change (Bryant & Kazan, 2012). Reynolds (2020) adopted the skills from the classic book How to Win Friends and Influence People and found these soft skills to improve a leader’s overall effectiveness. Impact is how intention and influence are measured (Bryant & Kazan, 2012). In an extensive review of literature on leadership published between 2008 and 2018, Hughes (2019) examined the measurable impact of nurse leaders on nursing staff and patient outcomes. She concluded that the most effective leadership strategies are those that have a well-established fit within the context of the organization and situations.
From Work-life Balance to Work-life Effectiveness
The concept of work-life effectiveness is not new. Work-life effectiveness is defined as a “specific set of organizational practices, policies, programs, and a philosophy that recommends aggressive support for the efforts of everyone who works to achieve success both at work and at home” (Alliance for Work-life Progress, 2005, p. 2). Doucette (2020) argues that achieving work-balance is a myth and is unattainable. Rather, one should focus on owning and defining what an effective work-life relationship should be. Chasing work-life balance may lead to more stress, whereas work-life effectiveness can change perceptions of leadership, relationships, and priorities. Ultimately, work-life effectiveness can increase one's sense of commitment and accomplishment (Doucette, 2020, p. 56). Work-life effectiveness covers a wide range of support systems including those that focus on individual effort and those the organization provides. These include work-life flexibility, paid and unpaid time-off, health and well-being, caring for dependents, financial support, community involvement, management involvement, and culture change interventions (Alliance for Work-life Progress, 2005).
There are No Leaders Like Nurse Leaders
Mary Ann Fuchs, president of the American Organization for Nursing Leadership, reminds us that "although it is frightening, there is no profession better equipped than nursing to lead through this pandemic (2020, p. 1)." I would echo this sentiment. As the Texas Organization for Nursing Leadership continues to reach out to its members, it is making strides in defining a nurse leader, different from any kind of other leaders. Goldsby et al. (2020) sum this up with these words: Few professionals in our society make more critical and important decisions than nurse managers. Often, the decisions they make are framed under "life or death" situations and they must do so in collaboration with and the full cooperation of their frontline staff. As such, nurse managers and leaders must be provided with the assistance and support they need.
Parting Words
New competencies have emerged in response to the current healthcare environment. These include the ability to lead through uncertainty, cultivate trust, and reskilling for the opportunity (Study: COVID creates a leadership gap, 2020). Manz (2015) urges us to aim for the self-leadership high road, which encompasses authenticity, responsibility, and increasing capacity. Ultimately, self-leadership enables and empowers nurse leaders to improve their performance and achieve their goals by clearly understanding their intentions, recognizing their impact, and harnessing their influence! As we work toward self-leadership, let us be reminded by the wisdom of Robert Frost (Poetry Foundation, 2020): “Two roads diverged in a wood, and I – I took the one less traveled by, and that has made all the difference.”
References
Abid, G., Arya, B., Arshad, A., Ahmed, S., & Farooqi, S. (2020). Positive personality traits and self-leadership in sustainable organizations: Mediating influence of thriving and moderating role of proactive personality. Sustainable Production and Consumption, 25, 299–311.
Alliance for Work-life Progress. (2005). The categories of work-life effectiveness. Retrieved from https://www.bestworkplaces.org/pdf/awlp/Categories%2520of%2520W-L%2520Effectiveness%2520Booklet%2520(final%252004.05).pdf
Ahmed, S. T. (2020). Managing news overload (MNO): The COVID-19 infodemic. Information (2078-2489), 11(8), 375.
Ay, F. A., Karakaya, A., & Yilmaz, K. (2015). Relations between self-leadership and critical thinking skills. Procedia - Social and Behavioral Sciences, 207, 29–41.
Bennis, W., & Nanus, B. (1985). Leaders: The strategies for taking charge. Harper & Row.
Bywater, J., & Lewis, J. (2019). Leadership: What competencies does it take to remain engaged as a leader in a VUCA world? Assessment & Development Matters, 11(3), 2–9.
Bryant, A., & Kazan, A. L. (2012). Self-leadership: How to become a more successful, efficient, and effective leader from the inside out (1st ed.). McGraw-Hill Education.
Cristofaro, M., & Giardino, P. L. (2020). Core self-evaluations, self-leadership, and the self-serving bias in managerial decision making: A laboratory experiment. Administrative Sciences (2076-3387), 10(3), 64. https://doi.org/10.3390/admsci10030064
Doucette, J. N. (2020). Achieving work-life effectiveness. Nursing Management, 51(10), 56. https://doi.org/10.1097/01.NUMA.0000698136.48144.fd
Fuchs, M. (2020). Best practices in pandemic response. Voice of Nursing Leadership, 18(5), 1.
Furtner, M. R., Tutzer, L., & Sachse, P. (2018). The mindful self-leader: Investigating the relationships between self-leadership and mindfulness. Social Behavior & Personality: An International Journal, 46(3), 353–360. https://doi.org/10.2224/sbp.6521
Goldsby, E., Goldsby, M., Neck, C. B., & Neck, C. P. (2020). Under pressure: Time management, self-leadership, and the nurse manager. Administrative Sciences (2076-3387), 10(3), 38. https://doi.org/10.3390/admsci10030038
Johansen, B. (2012). Leaders make the future: Ten new leadership skills for an uncertain world. Barrett-Koehler.
Kim, A.Y., & Sim, I.O. (2020). Mediating factors in nursing competency: A structural model analysis for nurses’ communication, self-leadership, self-efficacy, and nursing performance. International Journal of Environmental Research and Public Health, 17(6850), 1-14.
Lacey, S. R. (2020). An enduring crisis: Nurse leaders’ perspectives. Nursing Economic$, 38(5), 258–266.
Manz, C. C. (2015). Taking the self-leadership high road: Smooth surface or potholes ahead? Academy of Management Perspectives, 29(1), 132–151. https://doi.org/10.5465/amp.2013.0060
McDonald, D. (2019). Investigating intentionality and mindfulness of storytelling as pedagogy. Curriculum & Teaching Dialogue, 21(1/2), (Sp)97-(Sp)110.
Misra, S., Roberts, P., & Rhodes, M. (2020). Information overload, stress, and emergency managerial thinking. International Journal of Disaster Risk Reduction, 51. https://doi.org/10.1016/j.ijdrr.2020.101762
Poetry Foundation. (2020). The road not taken. Retrieved fromhttps://www.poetryfoundation.org/poems/44272/the-road-not-taken
Remegio, W., Rivera, R. R., Griffin, M. Q., & Fitzpatrick, J. J. (2020). The professional quality of life and work engagement of nurse leaders. Nurse Leader. https://doi.org/10.1016/j.mnl.2020.08.001
Reynolds, S. S. (2020). How to win friends and influence people—as a nursing leader. Nurse Leader. https://doi.org/10.1016/j.mnl.2020.07.013
Sahi, M. (2017). A study of self-leadership in relation to emotional competence and personality. International Research Journal of Management Science & Technology, 8(5). 281-289.
Stewart, G. L., Courtright, S. H., & Manz, C. C. (2019). Self-leadership: A paradoxical core of organizational behavior. Annual Review of Organizational Psychology and Organizational Behavior, 6, 47-67.
Study: COVID creates leadership gap. (2020). Leadership Briefings, 35, 1–8. Tuazon, N. (2020). Nurses’ response to COVID-19: A portrait of courage, collaboration, and co-creation. TONL Monthly. Retrieved from https://www.naylornetwork.com/tne-nwl/articles/index-v2.asp?aid=618160&issueID=74468
van Dorssen-Boog, P., De Jong, J., Veld, M., & Van Vuuren, T. (2020). Self-leadership among healthcare workers: A mediator for the effects of job autonomy on work engagement and health. Frontiers in Psychology, 11, 1420.
Filipino-American History Month-October
October is Filipino-American History Month!
It was a full house on October 10th 2020. On behalf of the The Philippine-American Chamber of Commerce Central Texas Region, we’d like to thank you all for celebrating Filipino-American History month. Not only did we have the the Filipino-American community in attendance, but also Asian-American Representatives from all over the state of Texas and beyond.
Next Battle Over Alamo Plan? Future of Woolworth Building & SA Civil Rights History
PACC board member Dr. Carey Latimore discusses the impact slavery, race, policing, and the Alamo in a News4SA interview with Randy Beamer - https://news4sanantonio.com/news/local/podcast-the-future-of-the-alamo-is-unclear-but-so-is-the-historical-woolworth-building
Equity: Creating a Leadership Culture Beyond Equality
Nelson Tuazon, DNP, DBA, RN, NEA-BC, CENP, CPHQ, CPPS, FNAP, FACHE
Vice President & Associate Chief Nursing Officer, University Health System, San Antonio
Director, District 8, Texas Organization for Nursing Leadership
Earlier in my career as a novice leader in healthcare management, one sage advice that my mentors emphasized was for me to treat everyone fairly and equally. As I advanced in my roles, I kept this advice as a core leadership principle. As a backdraft, in 2002, the Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care published its seminal work entitled, Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. This publication examined how disparities in treatment occurred in health care systems and explored the healthcare experience of persons of color (Smedley et al., 2003). The focus in this era of healthcare was on inequality. More than a decade and half later, the National Academies of Sciences, Engineering, and Medicine (2017) published a new report entitled, Communities in Action: Pathways to Health Equity. The focus shifted to health equity.
Health Equity: Completing the Triple Aim Equation
Misconceptions regarding equality and equity persist. The two terms are not the same and should not be used interchangeably. Over time, the term equality changed its meaning, and its emphasis focused on the similarity of treatment of individuals and groups. Equality refers to the process of treating everyone the same and falls short of taking into account the differences and needs of individuals or the context in which disparities occur (Walden et al., 2018). The concept of equality failed to convey the notion that not all individuals begin at the same starting point and became associated with norms of the dominant male, white, and middle class (Gosepath, 2011). Equity has become an alternative and linked to social justice. Although there are criticisms that special treatment may occur, equity addresses the social, economic, and political causes of inequality and offers remedies to prevent and avert disparate outcomes (Takeuchi et al., 2018).
Global Health and Equity. The concept of health equity has received global attention. The World Health Organization (WHO) defines health equity as the absence of unfair and avoidable differences in health interventions and outcomes among groups of people. The key element in this definition is focused on the opportunity for everyone to have the opportunity to attain their full health potential and that no one should be disadvantaged from achieving this potential (WHO, 2020, para. 1).
Focus on Health Equity in the US. The US Department of Health Human Services' 2018-2022 Strategic Plan integrates diversity, inclusion, and equity in five strategic goals particularly about improving access to healthcare, measuring and reporting on healthcare quality and disparities, and strengthening and expanding healthcare workforce to meet America’s diverse needs (Health and Human Services, 2019). The National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) of the Centers for Disease Control and Prevention (CDC) describes the achievement of health equity as the state by which every person has the opportunity to attain full health potential. The achievement of this potential should not pose any disadvantage to an individual due to social position or other socially determined circumstances (CDC, 2020, para. 1).
Health Inequities and Healthcare Disparities
Healthcare leaders, regulators, and various healthcare professionals across nations have raised the issue of inequities in health, particularly on the quality of healthcare and justice. The Institute for Healthcare Improvement (IHI, 2020) believes that healthcare inequities and disparities continue to exist. The differences in access to healthcare and treatment and the associated outcomes are systemic but are avoidable. Nurses are at the forefront and positioned to contribute to the achievement of healthcare equity. However, there is paucity of evidence to demonstrate that healthcare workers, particularly nurses, have propelled the concept of health equity (Estacio, 2019). In the workplace, biases related to stereotypes and gender roles persist despite the progress made towards workplace equality (Walden et al., 2018).
Addressing Health Equity in Academia. In its eleventh report to the Secretary of the Department of Health and Human Services and the Congress, the National Advisory Council on Nurse Education and Practice (NACNEP) reported the many successes towards the advances in nursing diversity in the US. However, NACNEP cautioned that the US healthcare workforce has not realized the goal of a healthcare workforce that reflects the diverse US population. Several barriers continue to exist including weak minority representations among faculty and in leadership roles in healthcare organizations and underrepresentation of students and applicants to educational institutions for healthcare professions (NACNEP, 2013). The National Education Progression in Nursing (NEPIN) has also examined the linkages between equity and academic achievement. NEPIN aims to ensure that nurses have access to higher levels of education and achievement (Aragon, 2020, para. 1).
Healthcare Organizations and Health Equity. US healthcare organizations that the Joint Commission (TJC) accredits and certifies are required to protect the rights of individuals and prohibit discrimination. TJC (2020) has posted guidelines and resources to assist TJC-accredited healthcare organizations in promoting racial justice and equity. Wyatt et al. (2016) offered a framework that healthcare organizations can follow to achieve health care equity. These authors wrote a white paper for the IHI that recommends guidance to reduce healthcare disparities related to racial and ethnic groups, religion, socio-economic status, gender, sexual orientation, age, mental health and other factors associated with discrimination or exclusion.
Social and Moral Determinants of Health. An understanding of the social determinants of health is critical in addressing health inequities and healthcare disparities effectively. Several screening tools have been developed including a) PREPARE: Protocol for Responding to and Assessing Patient Assets, Risks, and Experiences, b) the Social Needs Screening Tool, c) the Accountable Health Communities Health-Related Social Needs Screening Tool, and d) the Social Needs Screening Toolkit (Lathrop, 2020). Berwick (2020) challenges healthcare leaders to go beyond the social determinants of health and delve deeper into what he calls the moral determinants of health. His thought-provoking insights and questions compel us to think of ways to advocate for better health, beyond what he labels hospitals and physician offices as “repair shops.”
Call to Action
The literature offers several ideas to promote a culture of inclusion to influence and inspire nurses to be engaged in professional organizations (Tuazon, 2020). Walden et al. (2018) warned that emerging leaders and seasoned professionals should be aware of the impact of biases in the workplace and recognize how these biases affect the advancement of others and their own. As the Texas Organization for Nursing Leadership continues to advocate for diversity and inclusion, strategies to address equity complete the leadership equation.
Public Policy, Population Health, and Collaboration. To address health equity effectively, nurses must involve themselves and engage in policy development and implementation, promote population health, and forge interpersonal collaboration (Moss & Phillips, 2020). Nurses and nursing organizations must familiarize themselves with the work of the American Association of Retired Persons (AARP) Foundation, the AARP, and the Robert Wood Johnson Foundation (RWJF) on the Future of Nursing: Campaign for Action. The Campaign for Action’s (2020a) mantra explains its main thrust: “America’s 4 million nurses are key to improving health equity and creating communities in which everyone has access to high-quality care.” The American Organization for Nursing Leadership (AONL) is a member of the Campaign for Action’s Champion Nursing Council (Campaign for Action, 2020b).
Academic, Practice, and Research Partnership. NACNEP (2013) identified two primary recommendations to support the mission of eliminating health disparities. These include 1) promote nursing workforce diversity to achieve health equity, and 2) support effective decision-making and evaluation of diversity program outcomes. NEPIN suggests that organizations need to develop new programs strategically to improve diversity, equity, and inclusion and to promote cultural proficiency in teaching, research, service, and practice (Aragon, 2020).
Health Disparities and Health Inequities. The CDC, through the NCCDPHP, has published resources related to health equity and racial and ethnic disparities. These resources include a) REACH – Racial and Ethnic Approaches to Health, b) social determinants of health maps, c) surveillance systems, and d) addressing health disparities among youth (CDC, 2020).
Health Equity as a Strategic Priority. Mate and Wyatt (2017) urge health systems to put health equity as part of their strategic priorities. They offer the following recommendations: a) make health equity a leader-driven priority; b) develop structures and processes to support equity; c) take specific actions to address the social determinants of health; d) confront institutional racism within the organization, and e) partner with community organizations. Schoonover (2018) explains why health equity matters and offers ways to address health inequities effectively.
Final Thoughts
The discussion on equality and equity provokes intellectual debate but also evokes emotional responses. There is evidence in the literature that supports the conceptual and philosophical basis of promoting equity, rather than discussing equality in isolation. I submit that the Health Equity Framework proposed by Cohen et al. (2017) offers a logical and methodical approach. As the Texas Organization for Nursing Leadership (TONL) embarks upon strategies to address diversity, inclusion, and equity, it would behoove its leaders, through the proposed Taskforce on Diversity, Equity, and Inclusion, to utilize this framework. The following questions should inform and guide the proposed strategies: a) are the proposed programs, initiatives, or steps (means/process) following a fair and inclusive process, and b) are the desired targets and results (ends/outcomes) fair? The thoughtful, deliberate, and insightful answers to these questions will lead to solutions and approaches that create a culture of equity among all members, leaders, and stakeholders of the organization. Ultimately, equity in healthcare leads to high levels of organizational performance, promote value to all stakeholders, and sustain organizational excellence (Betancourt, 2020).
References
Aragon, S., Beauvais, A. Friday, V., Green, C., Kiger, A., King, S., Lear, T., Mahowald, J., McGuill, G., Perkins, D., Valdez, A., Velasco, B., & Wangerin, V. (2020). White paper: Equity, achievement and thriving in nursing education. National Education Progression in Nursing. https://nepincollaborative.org/white-paper-equity-achievement-and-thriving-in-nursing-education/
Berwick, D. (2020). The moral determinants of health. JAMA, 324(3), 225-226.
Betancourt, J. R. (2020). The path to equity in healthcare leads to high performance, value, and organizational excellence. Journal of Healthcare Management, 65(1), 7–10. https://doi.org/10.1097/JHM-D-19-00257
Campaign for Action (2020a). We’re building healthier communities through nursing. Retrieved from https://campaignforaction.org/
Campaign for Action (2020b). Nurses advance health equity and well-being for all. https://campaignforaction.org/nurses-advance-health-equity-and-well-being-for-all/
Cohen, A. B., Grogan, C. M., & Horwitt, J. N. (2017). The many roads toward achieving health equity. Journal of Health Politics, Policy & Law, 42(5), 739–748. https://doi.org/10.1215/03616878-3940414
Estacio, J. C. (2019). Health equity in nursing: A concept analysis. Nursing and Palliative Care International Journal, 2(1), 1-5. DOI: 10.30881/npcij.00008
Gosepath, S. (2007). Equality. The Stanford Encyclopedia of Philosophy. https://plato.stanford.edu/archives/spr2011/entries/equality/
Health and Human Services (HHS). (2019). Strategic plan FY 2018-2022. Retrieved from https://www.hhs.gov/about/strategic-plan/index.html?language=es
Institute for Healthcare Improvement (IHI). (2020). Health equity. Retrieved from http://www.ihi.org/Topics/Health-Equity/Pages/default.aspx
Lathrop, B. (2020). Moving toward health equity by addressing social determinants of health. Nursing for Women’s Health. doi: 10.1016/j.nwh.2019.11.003
Mate, K., & Wyatt, R. (2017). Health equity must be a strategic priority. Retrieved from https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0556
Moss, M., & Phillips, J. (2020). Health equity and nursing: Achieving equity through policy, population health and interpersonal collaboration. Springer.
National Academies of Sciences, Engineering, and Medicine. (2017). New report identifies root cause of health inequity in the US. Outlines solutions for communities to advance health equity. Retrieved from https://www.nationalacademies.org/news/2017/01/new-report-identifies-root-causes-of-health-inequity-in-the-us-outlines-solutions-for-communities-to-advance-health-equity
National Advisory Council on Nurse Education and Practice (NACNEP). (2013). Achieving health equity through nursing workforce diversity. Retrieved from https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/nursing/reports/2013-eleventhreport.pdf
Schoonover, H. (2018). Health equity: Why it matters and how to achieve it. Retrieved from https://www.healthcatalyst.com/health-equity-why-it-matters-how-to-achieve-it
Smedley, B., Stich, A., & Nelson, A. (2003). Unequal treatment: Confronting racial and ethnic disparities in health care. National Academies Press.
Takeuchi, D. T., Dearing, T. C., Bartholomew, M. W., & McRoy, R. G. (2018). Equality and equity:
Expanding opportunities to remedy disadvantage. Generations, 42(2), 13–19.
The Joint Commission (TJC). (2020). The Joint Commission stands for racial justice and equity. Retrieved from https://www.jointcommission.org/resources/news-and-multimedia/the-joint-commission-stands-for-racial-justice-and-equity/
Tuazon, N. (2020, August). Inclusive leadership: Influencing and inspiring professional organizational engagement. TONL Monthly. Retrieved from https://www.naylornetwork.com/tne-nwl/articles/index-v2.asp?aid=627039&issueID=74470
Walden, T., Snapp, H., Morgenstein, K., & Gregory, I. (2018). Starting the discussion about equality and equity in leadership. Audiology Today, 30(3), 36–47.
World Health Organization (WHO). (2020). Health equity. Retrieved from https://www.who.int/topics/health_equity/en/
Wyatt, R., Laderman, M., Botwinick, L., Mate, K., & Whittington, J. (2016). Achieving health equity: A guide for health care organizations. IHI White Paper. IHI.
*This article originally appeared in Tuazon, N. (2020, September). Equity: Creating a leadership culture beyond equality. TONL Monthly. Retrieved from https://www.naylornetwork.com/tne-nwl/articles/index-v2.asp?aid=631522&issueID=74471. Reprinted with permission.
2020 San Antonio Filipino-American Restaurant Census
On behalf of the Philippine American Chamber of Commerce, Central Texas Region, we would like to thank the Filipino-American community of San Antonio and surrounding areas for contributing to this census of Filipino owned restaurants. Our objective in collecting this is to bring awareness of the many small businesses that contribute to the diverse San Antonio economy. The Philippine American Chamber of Commerce supports entrepreneurship and continual community development and therefore will continue to update this list as often as necessary. Please contact Secretary and Public Media Relations Chair, Dominique Liu at dominique.liu@gmail.com for inquiries regarding this Census.
Yolanda Moy,
Region Chair
Philippine American Chamber of Commerce, Central Texas Region
2020 Filipino-American Restaurants in Alphabetical Order:
Bakery Lorraine
BBQ Done Wright
Fili-Deli
Filipino Express
Jeepney Street Eats
Just Lechon
Kain Na Filipino Cuisine
Malabito St. Inc.
Laguna Cafe
Lily’s Philippine Restaurant
Lumpia King
Pearl of the Orient
Sari-Sari Filipino Restaurant, Market & Bakery
Smashin Crab
Susie’s Lumpia
Tabares Filipino Restaurant
Pearl of the Orient
Sari-Sari Filipino Restaurant, Market & Bakery
Smashin Crab
Susie’s Lumpia
Tabares Filipino Restaurant
Prepared by Dominique Liu
Secretary and Public Media Relations Officer
Inclusive Leadership: Influencing and Inspiring Professional Organizational Engagement
By Nelson Tuazon, DNP, DBA, RN, NEA-BC, CENP, CPPS, CPHQ, FNAP, FACHE
Vice-President & Associate Chief Nursing Officer, University Health System, San Antonio, Texas
District 8 Director, Texas Organization for Nursing Leadership
The U.S. workplace continues to undergo a demographic change at a rapid pace. The composition of the workforce will be impacted by the increasing number of Asian and Hispanic workers and professionals. The growth of Black Americans is projected to be 6.4 million by 2050. Whites make up the majority of the labor force (78%), Blacks (13%), and Asians (6%). By ethnicity, 17% of the labor force were of Hispanic or Latino ethnicity, who may be of any race (Bureau of Labor Statistics, 2018). By 2025, racial and minority groups will comprise 42% of the U.S. population, thereby increasing the diversity of the workforce (Brimhall et al., 2014). The rapid shifts in the U.S. workforce demographics have provided the impetus for organizations to forge culturally competent labor force and develop inclusive work environments (Velasco & Sansone, 2019).
What Is in a Name?
The terms diversity and inclusion have been used interchangeably; however, it is important to differentiate the two. Diversity refers to the presence of people possessing a wide range of characteristics, which may be seen and unseen, and which the members were born or acquired. Inclusion, on the other hand, refers to the practice of making all members feel welcomed and providing them with an atmosphere that provides equal opportunity to connect, belong, and grow (Fucci & Cooper, 2019). Diversity also refers to the composition of differences of individuals, which traditionally may include race, ethnicity, gender, and education (Homan & Greer, 2013). Inclusion, on the other hand, refers to the extent to which the members of the group are encouraged and urged to participate and get involved (Mor Barak, 2015). The ultimate aim of inclusion is to value the characteristics of the individual members and to foster a welcoming climate that promotes the sharing of their true selves (Nishii, 2013). Inclusive leadership is associated with the integration of diversity dimensions in leadership theory and is concerned with the knowledge of how these dimensions influence an understanding of leadership. Ultimately, inclusive leaders focus on the mechanism by which their followers view the leadership development of their leaders (Gotsis & Grimani, 2016).
Why are Diversity and Inclusion Important?
Fucci and Cooper (2019) emphasized the importance of diversity and inclusion in corporate and nonprofit boards. Diversity and inclusion have been proposed as the possible key to overcoming the next recessions because they serve as a potent source of strength during tough times (Gencler, 2019). The 2020 McKinsey report indicates, however, that diversity does not always mean inclusion. Despite the increasing diversity, many companies are still unable to cultivate work environments that promote inclusive leadership and accountability. Equality and fairness to opportunities and freedom from bias and discrimination remain as issues (Gassam, 2020).
The business case for diversity and inclusion has been successfully demonstrated. Organizations with a clear purpose and intention of promoting diversity and inclusion should understand the current state of its workforce to have sustainable outcomes (Prieto et al., 2016). Diversity in the workforce has been linked to the achievement of better health care outcomes and more culturally appropriate and relevant care, for both the organizations and the communities they serve (Persaud, 2020). The formal assignment of responsibility for diversity to a diversity manager, taskforce, or committee has proved to be successful (Dobbin & Kaley, 2016).
There is evidence to show the benefits of an inclusive climate, especially in organizations that comprise diverse groups. The positive outcomes that have been associated with inclusive settings and organizations include member satisfaction, retention, engagement, creativity, and innovation (Bradley, 2020; Brimhall et al., 2014; Nishii, 2013). The McKinsey 2020 report indicates that gender diversity and ethnic and cultural diversity are associated with above-average profitability. Companies that subscribe to gender diversity are 25% more likely to be profitable and those that espouse ethnic and cultural diversity are 36% more likely to be profitable (Gassam, 2020). Increased profitability and innovation have been shown in companies that have greater diversity in their workforce and promote inclusion (Hunt et al., 2015).
Frameworks and Considerations for Diversity and Inclusion
One of the first important steps in developing strategies to integrate diversity and inclusion into the organization is the identification of a framework. Several theories and models exist in the literature. Some of the more fitting theories and models are presented here for consideration.
Social Identity Theory and Optimal Distinctiveness Theory
In examining the impact of inclusion on the leader-member exchange, Brimhall et al. (2017) analyzed theoretical frameworks that may be used. They explored the social identity theory (Tajfel, 1982) and the optimal distinctiveness theory (Brewer, 1991). Brimhall et al. (2017) posited that being part of a group, trust, and feelings of acceptance promote the feelings of inclusion. An important aspect of inclusion, beyond the feeling of belonging to a group, is the sense of being valued and accepted for the unique characteristics an individual brings to the group (Mor Barak, 2015; Nishii, 2013).
Humanitarianism
Harpell and Andrews (2010) offered humanitarianism as a framework, which regards all humans as equal. Broadly, humanitarianism aligns with diversity and inclusion because of its focus on fair treatment and respect for all individuals. Although Harpell and Andrews focused on the application of inclusion in the academic arena, their exposition on the individual needs of the learners and the need to adjust the instructional methods to meet the needs of the students, apply to the inclusion roles of leaders of professional organizations towards their members.
Social Change Model
The social change model (SCM) promotes equity, social justice, self-knowledge, service, and collaboration. This model is particularly relevant to individuals who may not perceive themselves as leaders and is especially meaningful in a diverse society (Read et al., 2015, p.164). The seven values of SCM encompass the individual (consciousness of self and others, congruence, commitment), group (collaboration, common purpose, controversy with civility), and society (citizenship). SCM aligns with inclusive leadership because the model promotes equity, social justice, self-knowledge, service, and collaboration (Read et al., 2015, p. 166).
Organizational Culture
Sanders (2017) has explored the concepts of organizational culture as a framework for integrating diversity and inclusion. The Organizational Culture Assessment Instrument (OCAI) (Cameron & Quins, 2011), based on the competing values framework, is a fitting model in examining diversity and inclusion because of its flexibility and adaptability. The application of OCAI is suitable for diversity and inclusion mainly due to the assumption that there is no one best culture; rather, the model is premised on the notion that cultures vary based on circumstances (Sanders, 2017).
Faultlines
Organizations, institutions, and professional associations are continuing to attract employees, clients, patients, and members from diverse backgrounds. In response, organizations form interprofessional health care teams to address the multifaceted issues resulting from the increasingly complex interplay of factors affecting these entities. Adding to the complexity of group interaction and the success of teams is the concept of faultlines (Mitchell & Boyle, 2020). Faultlines are the hypothetical separations and distinctions that segregate teams into subgroups based on their attributes and characteristics (Lau & Murnighan, 1998). The composition of teams is a major factor that is linked to team dynamics and performance (Mitchell & Boyle, 2015). In the case of professional associations such as the Texas Organization for Nursing Leadership (TONL), there may be perceived faultlines amongst the members from various settings such as the acute care, academic setting, and post-acute care. There may also be a division in the professional roles of the members such as those who are nurse executives, directors, and managers and those who are at the beginning of their leadership roles as supervisors.
Although faultlines are viewed as negative due to the effect of conflicts to group performance (Lau & Murnighan, 1998), there is an alternative view to argue that faultlines could be beneficial especially when the diverse team is working to solve complex problems and propose innovative solutions (Mitchell & Boyle, 2015). Academic-practice partnership is an example of an approach where diverse teams solve complex problems. Inclusive leadership can promote and foster the sharing of diverse input from the different team members with unique capabilities. The synergy, collaboration, and combined effort from the interprofessional team could enhance innovation. The presence of strong faultlines will lead to a greater likelihood of the emergence of interprofessional comparative dynamics (Carton & Cummings, 2013).
Who is an Inclusive Leader?
Six Signature Traits of Inclusive Leaders
Inclusive leaders have the following characteristics: a) visible commitment – a commitment to and making diversity and inclusion a priority; b) humility and courage – modesty, admission of culpability, and valuing others’ contributions; c) awareness of bias or cognizance – awareness of personal blind spots; d) curiosity about others – open-mindedness and non-judgmental attitude; e) cultural intelligence – cultural awareness and adaptability, and f) effective collaboration – empowering others and promoting psychological safety (Bourke & Dillon, 2016; Bourke & Espedido, 2019; Bourke & Espedido, 2020). Tapia and Polonskaia (n.d., p. 9) describe inclusive leaders with the following traits: a) authenticity – humility, setting aside ego, and establishing trust; b) emotional resilience – composure amidst adversity and differences; c) self-assurance – confidence and optimism; d) inquisitiveness – openness, curiosity, and empathy; and e) flexibility – tolerance to ambiguity and adaptability.
Commitment, Connection, and Collaboration
Inclusive leaders commit to making diversity and inclusion as an organizational priority by engaging all levels of management and staff in the organization, developing formal processes and structures to create a positive work environment, and engaging employees from various backgrounds. Inclusive leaders make connections with individuals early and engage them in a continuous process of leadership development. Specific criteria and clear pathways are developed and communicated to diverse groups at the entry- mid- and senior levels within the organization. Finally, inclusive leaders collaborate with external stakeholders towards the achievement of shared goals to promote equity and create the momentum for diversity among the leadership team (Persaud, 2020).
What are the Competencies of an Inclusive Leader?
Inclusive leadership requires specific skills and competencies in effective communication. When communicating with others, particularly in a cross-cultural and diverse group, inclusive leaders convey the message of being included, valued, and heard. The ability to bring individuals from different backgrounds to a common platform characterizes an inclusive leader (Jain, 2018). The role of servant leadership has been examined as an approach to fostering inclusion. Gotsis and Grimani (2016) have identified organizations that promote the perceptions of employees of inclusion. Through empowerment, diverse groups perceive equitable and more humane work climates. Servant leaders are believed to be more sensitive to different societal expectations.
Inclusive leaders should develop and master the following competencies: a) build interpersonal trust, b) integrate diverse perspectives; c) optimize talent; d) apply an adaptive mindset; and e) achieve transformation (Tapia & Polonskaia, n.d., p. 10). Additionally, inclusive leaders can adopt the following strategies in promoting organizational change that fosters diversity and inclusion: a) lean into discomfort – this opens the door to trust; b) listen as an ally – this opens the door to collaboration; c) state your intent and your intensity – this opens the door to understanding; and d) share your street corner – this opens the door to breakthroughs (Sanders, 2017, pp.77-78). It is important to remember that organizational commitment to diversity and inclusion does not mandate leaders to hire or promote unqualified individuals for leadership roles or positions (Persaud, 2020).
How Do the Leading Professional Organizations Embody Diversity and Inclusion?
A review of the websites of six major leadership and executive organizations revealed three primary approaches to diversity and inclusion. These include structures (e.g. committees, councils, expert panels, and institutes), representation (e.g. policy statement, forums, recruitment, and retention), recognition (e.g. awards, research, publications, and celebration). These organizations include the American Academy of Nursing (AAN), American Association of Colleges of Nursing (AACN), American Nurses Association (ANA), American Organization for Nursing Leadership (AONL), National League for Nursing (NLN), and the American College of Healthcare Executives (ACHE).
American Academy of Nursing
The American Academy of Nursing (AAN) has a Diversity and Inclusivity as the top values in its 2017-2020 Strategic Plan. The AAN has a Diversity and Inclusivity Statement that is aligned with its mission statement. The AAN a) requires its members to reflect the increasingly diverse society and their contributions across nursing; b) offers opportunities to engage the members in its work; and c) develops and aligns policies and policies to achieve goals. The AAN has expert panels that address diversity and inclusion. These include the expert panels on aging, cultural competence and health equity, lesbian, gay, bisexual, transgender, queer (LGBTQ) health, and women’s health (AAN, 2015).
American Association of Colleges of Nursing
The American Association of Colleges of Nursing (AACN) website features a Diversity and Inclusion page that highlights the organization’s rich resources including its comprehensive position statement, Diversity, Inclusion, & Equity in Academic Nursing (AACN, 2017). The page includes information on the Diversity in Nursing Education Award; data, publications, and educational programs on diversity; pod casts including topics on diversity in nursing education; and funding opportunities that provide resources to students, including many minority focused programs. The Diversity Digest newsletter, produced quarterly, highlights AACN’s diversity and inclusion initiatives. The Diversity in the News showcases current noteworthy announcements on diversity, inclusion, and equity (AACN, 2020). AACN is holding a Diversity Symposium entitled Diversity: Essential for Inclusive Excellence in December 2020.
American Nurses Association
The American Nurses Association (ANA) website features a Practice and Advocacy page that includes Diversity Awareness, an expansion from ANA’s Nursing’s Social Policy Statement. The page also highlights information and resources regarding LGBT Individuals and Communities, Racial and Ethnic Minority Communities, and Culturally-Specific Tools. The tools include resources about Black and African Americans, American Indian/Native Americans/Alaskan Natives, Asian and Pacific Islander Americans, and Hispanic and Latino Americans (ANA, n.d.a). ANA offers a Minority Fellowship Program that focuses on mental health and substance abuse (ANA, n.d.b).
American Organization for Nursing Leadership
The American Organization for Nursing Leadership (AONL) has a Diversity and Inclusion page, part of the Institute for Diversity and Health Equity of the American Hospital Association. The site has resources that include a Workforce Library and highlights Reports on the Guiding Principles for Diversity in Healthcare Organizations and Guiding Principles for Nurse Leaders. AONL features a Nurses’ Diversity, Equity and Inclusivity Pledge that it developed in partnership with the New England Regional Black Nurses Association (NERBNA). There is an Equity of Care Award that recognizes member hospitals and health systems for their efforts to advance diversity, inclusion, and equity (AONL, 2020).
American College of Healthcare Executives
The American College of Healthcare Executives (ACHE) webpage highlights its Diversity and Inclusion activities and initiatives that include a statement, “we are promoters of diversity and inclusion.” The page also showcases the LGBTQ Forum and the Asian Healthcare Leaders Forum, the ACHE Statement on Diversity, Research on Diversity, and the Policy Statements on Diversity (ACHE, 2020a). The Diversity and Inclusion Career Center features the Executive Diversity Career Navigator, the Thomas C. Dolan Executive Diversity Program, and Gender and Race/Ethnicity Studies (ACHE, 2020b). ACHE’s policy statement on Increasing and Sustaining Racial/Ethnic Diversity in Healthcare Management emphasizes its advocacy efforts to providing equal opportunity for all citizens regardless of race and ethnicity. The policy encompasses recruitment, promotion, and support for improving the representation and equitable treatment of racial and ethnic diversity in healthcare management (ACHE, 2020c).
National League for Nursing
The National League for Nursing (NLN) Advocacy and Public Policy page highlights its commitment to promote a population of nurses and nurse educators who reflect the diversity in the nation, advocate for policies that enrich culturally relevant nursing education, and support the incorporation of the national standards for Culturally and Linguistically Appropriate Services (CLAS) (NLN, 2020a). The NLN website also features a Diversity page that focuses on health disparities (NLN, 2020b). NLN’s Center for Diversity and Global Initiative has developed a comprehensive Diversity and Inclusion Toolkit that covers diversity and inclusivity in the academic mission, administrative leadership, faculty, and students (NLN, 2020c).
Strategies for Inclusive Leaders
Leaders could enhance their potential as an inclusive leader in their style and approach by adopting the following strategies (Dow, 2017). These include a) exemplify self-awareness; b) develop a strategy for leading; c) model courage; d) inspire trust and respect; e) exhibit self-control, and f) stop assigning blame. As leaders of professional organizations, we have to reflect upon these strategies that could affect our decision-making, ability to achieve organizational goals and objectives, inspire others to act with courage, build trust, and demonstrate emotional intelligence. As change agents, transformational leaders elevate individual and group performance by empowering others, holding individuals accountable, and adhering to diversity and inclusion (Davalos, 2014). Leaders that subscribe to transformative leadership theory focus on inclusion, equity, and social justice (Shields & Hesbol, 2020). It has been suggested that leadership theories should encompass social equity and inclusion issues that evolve as consequences of the rapid changes within the organization and the society (Chin, 2010).
To prepare early careerists and activists in the labor union movement, Alvarez and Alvarez (2018) shared the principles they developed to guide the young leaders to tackle the issues of racial and gender equity. Some of these include strategic recruitment of targeted diverse demographics, promoting the value of a learning community, developing leadership program focused on strategic thinking and broader issues rather than skills, and utilizing interactive pedagogy with peer learning and focused on self-assessments. Two principles that may sound like a shift from the inclusive leadership paradigm suggest that there should be a recruitment of internal candidates rather than self-selection and acceptance to the leadership training program should be selective. The implications of these principles to professional organizations are profound, particularly for students and young members who have the desire to be engaged in professional organizations. The following are some ideas to ponder upon.
a. To ensure that the demographic make-up of the organization is represented equally and equitably, appointed positions to the board, committees, and taskforces provides the leaders to offer opportunities to qualified candidates and nominees.
b. To create a pool of diverse candidates and nominees for elected and appointed positions, a succession planning committee should be established in addition to the nomination and election committee.
c. To create robust local and regional activities, strengthen the role and participation of the board members-at-large and the district directors.
d. To develop strategic agility and strategic thinking among the members, program development and educational offerings should be strategic in scope and scale.
e. To promote member engagement, deploy pedagogical approaches that cater to the various learning styles of individuals and that are based on identified learning needs.
Parting Words
The mission of nursing is profoundly aligned with social justice and health equity (Read et al., 2015). As advocates for social change, leaders of professional organizations are duty-bound to cultivate, foster, and advance diversity and inclusion among its members, constituents, and stakeholders. The creation of a culture of inclusion requires a new set of leadership qualities and competencies that include flexibility, fluidity, self-awareness and mindfulness, courage, and vulnerability (Wasserman et al., 2008, p. 180). Inclusion forges an environment that recognizes, espouses, and adopts various ways and experiences that allow individuals to reach their full potential and ultimately result in positive outcomes (Winters, 2014). Tapia and Poloskaia (n.d., p. 5) sum it best: "being an inclusive leader does not make you a good leader of inclusion and diversity – it makes you a good leader overall."
References
Alvarez, S. M., & Alvarez, J. F. (2018). Leadership development as a driver of equity and inclusion. Work & Occupations, 45(4), 501–528. https://doi.org/10.1177/07308884187863377
American Academy of Nursing (AAN). (2015). About. Retrieved from https://www.aannet.org/about/about-the-academy/diversity-statement
American Association of Colleges of Nursing (AACN). (2017). Diversity, inclusion, & equity in academic nursing. Retrieved from https://www.aacnnursing.org/Diversity-Inclusion/Publications-on-Diversity/Position-Statement
American Association of Colleges of Nursing (AACN). (2020). Diversity & inclusion. Retrieved from https://www.aacnnursing.org/Diversity
American College of Healthcare Executives (ACHE). (2020a). Diversity and inclusion. Retrieved from https://www.ache.org/about-ache/our-story/diversity-and-inclusion
American College of Healthcare Executives (ACHE). (2020b). Tools and resources: Diversity and inclusion career resources. Retrieved from https://www.ache.org/career-resource-center/special-groups/diversity-career-resources
American College of Healthcare Executives (ACHE). 2020c). Increasing and sustaining racial/ethnic diversity in healthcare management. Retrieved from https://www.ache.org/about-ache/our-story/our-commitments/policy-statements/increasing-and-sustaining-racial-diversity-in-healthcare-management
American Nurses Association (ANA). (n.d.a). Diversity awareness. Retrieved from https://www.nursingworld.org/practice-policy/workforce/clinical-practice-material/diversity-awareness/
American Nurses Association (ANA). (n.d.b). Minority Fellowship Program. Retrieved from https://www.nursingworld.org/practice-policy/workforce/minority-fellowship-program/
American Organization for Nursing Leadership (AONL). (2020). Diversity and inclusion. Retrieved from https://www.aonl.org/resources/diversity-and-inclusion
Bourke, J., & Dillon, B. (April 2016). The six signature traits of inclusive leaders: Thriving in a diverse new world. Retrieved from https://www2.deloitte.com/us/en/insights/topics/talent/six-signature-traits-of-inclusive-leadership.html
Bourke, J., & Espedido, A. (March 2019). Why inclusive leaders are good for organizations, and how to become one. Harvard Business Review. Retrieved from https://hbr.org/2019/03/why-inclusive-leaders-are-good-for-organizations-and-how-to-become-one
Bourke, J., & Espedido, A. (March 2020). The key to inclusive leadership. Harvard Business Review. Retrieved from https://hbr.org/2020/03/the-key-to-inclusive-leadership
Bradley, E. H. (2020). Diversity, inclusive leadership, and health outcomes. International Journal of Health Policy & Management, 9(7), 266.
Brewer, M. B. (1991). The social self: On being the same and different at the same time. Personality and Social Psychology Bulletin, 17, 475-482.
Brimhall, K. C., Lizano, E. L., & Mor Barak, M. E. (2014). The mediating role of inclusion: A longitudinal study of the effects of leader-member exchange and diversity climate on job satisfaction and intention to leave among child welfare workers. Children and Youth Services Review, 40, 79–88. https://doi.org/10.1016/j.childyouth.2014.03.003
Brimhall, K. C., Mor Barak, M. E., Hurlburt, M., McArdle, J. J., Palinkas, L., & Henwood, B. (2017). Increasing workplace inclusion: The promise of leader-member exchange. Human Service Organizations: Management, Leadership & Governance, 41(3), 222–239. https://doi.org/10.1080/23303131.2016.1251522
Bureau of Labor Statistics (2018). Labor force characteristics by race and ethnicity, 2018. Retrieved from https://www.bls.gov/opub/reports/race-and-ethnicity/2018/home.htm
Carton, A. M., & Cummings, J. N. (2013). The impact of subgroup type and subgroup configurational properties on work team performance. Journal of Applied Psychology, 98(5), 732-758.
Chin, J. L. (2010). Introduction to the special issue on diversity and leadership. American Psychologist, 65(3), 150-156.
Davalos, C. D. (2014). The role of chief diversity officers in institutionalizing diversity and inclusion: A multiple case study of three exemplar universities. Proquest Digital Dissertation, 3581650.
Dow, C. (2017). It starts by picking up a mirror: An introspective look at inclusive leadership. Armed Forces Comptroller, 62(4), 21–23.
Fucci, M., & Cooper, T. (April 2019). The inclusion for boards: Redefining board responsibilities to support organizational inclusion. Retrieved from https://www2.deloitte.com/us/en/insights/topics/value-of-diversity-and-inclusion/redefining-board-responsibilities-to-support-organizational-inclusion.html
Gencler, D. (December 2019). New study reveals that diversity and inclusion may be the key to beating the next recession. Retrieved from https://www.msn.com/en-us/money/other/new-study-reveals-that-diversity-and-inclusion-may-be-the-key-to-beating-the-next-recession/ar-BB16N5FM
Gassam, J. (May 2020). McKinsey new report finds that diversity does not equal inclusion. Retrieved from https://www.forbes.com/sites/janicegassam/2020/05/19/mckinseys-new-report-finds-that-diversity-does-not-equal-inclusion/#ed346b87066b
Gotsis, G., & Grimani, K. (2016). The role of servant leadership in fostering inclusive organizations. Journal of Management Development, 35(8), 985.
Homan, A. C., & Greer, L. L. (2013). Considering diversity: The positive effects of considerate leadership in diverse teams. Group Processes & Intergroup Relations, 16(1), 105–125. https://doi.org/10.1177/1368430212437798
Hunt, V., Layton, D., & Prince, S. (January 2015). Why diversity matters. Retrieved from https://www.mckinsey.com/~/media/McKinsey/Business%20Functions/Organization/Our%20Insights/Why%20diversity%20matters/Why%20diversity%20matters.pdf
Jain, N. (2018). Inclusive leadership and effective communication: An unbreakable bond. Language in India, 18(12), 207–215.
Lau, D., & Murnighan, J. K. (1998). Demographic diversity and faultlines; the compositional dynamics of organizational groups. Academy of Management Review, 23(2), 325-340.
Mitchell, R., & Boyle, B. (2015). Professional diversity, identify salience and team innovation: The moderating role of openmindedness norms. Journal of Organizational Behavior,36(6), 873-894.
Mitchell, R., & Boyle, B. (2020). Professional faultlines and interprofessional differentiation in multidisciplinary team innovation: The moderating role of inclusive leadership. Health Care Management Review. https://doi.org/10.1097/HMR.0000000000000276
Mor Barak, M. E. (2015). Inclusion is the key to diversity management, but what is inclusion? Human Service Organizations: Management, Leadership & Governance, 39(2), 83–88. https://doi.org/10.1080/23303131.2015.1035599
National League for Nursing (NLN). (2020a). Advocacy and public policy. Retrieved from http://www.nln.org/advocacy-public-policy/legislative-issues/diversity
National League for Nursing (NLN). (2020b). Diversity. Retrieved from http://www.nln.org/advocacy-public-policy/issues/diversity
National League for Nursing (NLN). (2020b). Diversity toolkit. Retrieved from http://www.nln.org/professional-development-programs/teaching-resources/toolkits/diversity
Nishii, L. H. (2013). The benefits of climate for inclusion for gender-diverse groups. Academy of Management Journal, 56(6), 1754–1774. https://doi.org/10.5465/amj.2009.0823
Persaud, S. (2020). Diversifying nursing leadership through commitment, connection, and collaboration. Nursing Administration Quarterly, 44(3), 244–250. https://doi.org/10.1097/NAQ.0000000000000422
Prieto, L. C., Norman, M. V., Phipps, S. T. A., & Chenault, E. B. S. (2016). Tackling micro-aggressions in organizations: A broken windows approach. Journal of Leadership, Accountability, and Ethics: Lighthouse Point, 13(3), 36-49.
Read, C. Y., Pino Betancourt, D. M., & Morrison, C. (2016). Social change: A framework for inclusive leadership development in nursing education. The Journal of Nursing Education, 55(3), 164–167. https://doi.org/10.3928/01484834-20160216-08
Sanders, E. J. (2017). The human frontier: Building an inclusive organizational culture. Journal of Organizational Psychology, 17(1), 71–82.
Shields, C. M., & Hesbol, K. A. (2020). Transformative leadership approaches to inclusion, equity, and social justice. Journal of School Leadership, 30(1), 3. https://search.ebscohost.com/login.aspx?direct=true&db=edb&AN=140273914&site=eds-live&scope=site
Tajfel, H. (1982). Social psychology of intergroup relations. Annual Review of Psychology, 33, 1-39.
Tapia A., & Polonskaia, A. (n.d.). The 5 disciplines of including leaders: Unleashing the power of all of us. Korn Ferry. Retrieved from https://infokf.kornferry.com/rs/494-VUC-482/images/Korn-Ferry-The-Inclusive-Leader-5-Disciplines.pdf
Velasco, M., & Sansone, C. (2019). Resistance to diversity and inclusion change initiatives: Strategies for transformational leaders. Organization Development Journal, 37(3), 9–20.
Wasserman, J. C., Gallegos, P. V., & Ferdman, B. M. (2008). Dancing with resistance: Leadership challenges in fostering a culture of inclusion. In Thomas, K. M. (Ed.), Diversity resistance in organizations (pp 175-200). Earlbaum.
Winters, M. (2014). From diversity to inclusion: An inclusion equation. In Ferdman, B. M. and Deane, B. R. (Eds.), Diversity at work: The practice of inclusion (pp. 205-228). Wiley-Blackwell.
FILCON's Kalayaan 2020
Celebrate Philippine Independence Day with "FilCon Kalayaan 2020" and TFC Hour — with your host, Gelo, and our special guest, Inigo Pascual! - https://www.facebook.com/permalink.php?story_fbid=976281749554181&id=337741936741502
Philippine Independence Day Celebration
Celebrate Philippine Independence Day with "FilCon Kalayaan 2020" and TFC Hour — with your host, Gelo, and our special guest, Inigo Pascual! - https://www.facebook.com/permalink.php?story_fbid=976281749554181&id=337741936741502
COVID-19 Update
COVID-19 UPDATE:
Good evening, San Antonio.
The below totals include 21 positive cases from Sunday.
Our current hospitalization numbers have ticked up a bit from last week.
We're now at 3333 (+22) cases:
From Mayor Ron Nirenberg
COVID-19 UPDATE:
Good evening, San Antonio.
The below totals include 21 positive cases from Sunday.
Our current hospitalization numbers have ticked up a bit from last week.
We're now at 3333 (+22) cases:
- 2332 are from the general public (+4)
- 410 are jail inmates (+0)
- 60 are jail staff (+0)
- 351 (+1) are from other congregate settings
- 180 (+17) remain under investigation
- 2077 individuals have fully recovered, 1156 remain ill
- 96 patients are currently hospitalized, 38 are in the ICU, 23 are on ventilators
~47% of our total cases are folks under 40 years old. Even if you feel fine, please be mindful of how this disease might affect more vulnerable loved ones and neighbors.
Progress warnings & indicators: https://covid19.sanantonio.gov/About-COVID-19/Dashboards-Data/Progress-Warning-Indicators
We are able to confirm receipt of 76,308 test results in Bexar County.
We are reporting no new deaths today.
Please note: Some cases under investigation from previous days were officially classified today, so the total jump in some categories may be higher than the number in parentheses.
---------
VENTILATORS / HOSPITAL BEDS:
1488 of 4706 staffed beds available, 32%. 96 are being used to fight COVID-19.
553 of 704 ventilators available, 79%. 23 are being used to fight COVID-19.
---------
The live nightly briefings with Judge Wolff will now occur on Tuesdays & Thursdays as we move into our Watch, Expand and Assure phase of COVID-19.
Data will still be updated daily on the COVID-19 website.
Learn more about the next phase here: https://covid19.sanantonio.gov/What-YOU-Can-Do/Reopening-Safely/WATCH-EXPAND-and-ASSURE-Plan
---------
If you've been at a demonstration, or even at a store that seemed too crowded, get tested! You don't need symptoms.
Call our hotline at 210-207-5779 to schedule a no-cost diagnostic test.
Monday- Friday: 8:00 a.m. to 4:00 p.m.
Saturday-Sunday: 8:00 a.m. to 12:00 p.m.
---------
We have a COVID-19 Emergency Housing Assistance Program, funded with $25 million from various sources.
Residents seeking assistance should visit: https://sanantonio.gov/EmergencyHousingAssistance or call 311
Text HousingHelpSA to 41444 to donate to this fund.
---------
COMMUNICATION PORTALS:
San Antonio COVID-19 website:
https://covid19.sanantonio.gov
American Sign Language:
http://sat.ahasalerts.com/ActiveAlerts.aspx?id=1334
COVID-19 Hotline: 210.207.5779
Text COSAGOV to 55000 for text alerts
Ready South Texas app:
https://readysouthtexasapp.com
---------
COVID-19 is still in our community.
Wash your hands. Practice physical distancing. Wear a mask. Please be careful if you need to travel to a public space.
Thank you, San Antonio
Support Mayor Ron Nirenberg’s 50,000 Masks Campaign!
Our Humanitarian Chairman, Dr. Nelson Tuazon, delivered 800 masks on behalf of the Philippine American Chamber of Commerce to support Mayor Ron Nirenberg’s 50,000 Masks Campaign! This initiative is a testament to our commitment to fostering entrepreneurship among Filipinos, Filipino-Americans, and their friends. By actively promoting business growth and supporting our communities, we play a vital role in enhancing economic development and professional opportunities.
Through our participation in this campaign, we aim to bolster trade, investments, and tourism between the Philippines and the United States. Our efforts not only contribute to the health and safety of our local community but also serve as a reminder of the enduring partnership and mutual benefits that stem from strong economic relations. Together, we can build a brighter and more prosperous future for everyone involved.
Testing
USS TELESFORO TRINIDAD CAMPAIGN
USS TELESFORO TRINIDAD CAMPAIGN (USSTTC)
“Ship and Shipmate Before Self”
MISSION: Name a US Navy Warship (Destroyer--DDG or Frigate--FFG) after Fireman Second Class Telesforo Trinidad, an American national of Filipino descent who received the Medal of Honor on April 1, 1915, for extraordinary heroism and intrepidity in the line of his profession to memorialize his heroic contributions to the U.S. Navy and our grateful Nation.
VISION: Perpetuate PO2 Trinidad’s heroic contributions to promote national awareness and education and bring pride and honor to the US Navy, its Sailors – officer and enlisted, their families and our Republic.
WHO WE ARE: USSTTC is a national grass roots advocacy group comprised of serving and retired members of the US Armed Forces, community leaders, academics, corporate executives, civic leaders, partners and sponsors, and veterans’ families committed to naming a US Navy Warship after Trinidad. (A 501(c)(3) application is in progress).
BACKGROUND: No US Navy ship has been named after a member of the US Armed Forces of Filipino descent, even though tens of thousands of Filipinos have served faithfully in the US Navy beginning in 1901 when President William McKinley signed an Executive Order allowing the Navy to enlist 500 Filipinos as part of the Insular Force. Approximately 6,000 Filipinos enlisted in the US Navy during WWI and many more joined through the interwar period leading up to WWII. After the Philippines obtained its independence from the United States in 1946, over 35,000 Filipinos were recruited into the US Navy from 1952 to 1992 under a provision of the Republic of the Philippines- United States Military Bases Agreement. In addition, thousands of Americans of Filipino descent enlisted during this same 40-year period, and continue to do so until today.
DISCUSSION: Trinidad remains the first and only American of Asian descent and first American national of Filipino descent in the US Navy to receive a Medal of Honor for his extraordinary heroism in the line of his profession during boiler explosions onboard the USS San Diego (ACR-6) while the ship was underway in the Gulf of California on January 21, 1915. Trinidad brought two crewmembers to safety in spite of his own physical injuries from the explosion. He was awarded the Medal of Honor in accordance with General Order Number 142 signed by the Secretary of the Navy Josephus Daniels on April 1, 1915.
To date, there is only one ship, the USS Chung-Hoon (DDG-93) named after an Asian American in the Navy - Rear Admiral Gordon Pai’ea Chung-Hoon, Commanding Officer of USS Sigsbee (DD-502) during World War II, who received the Navy Cross for his gallant actions during a kamikaze attack on April 14, 1945.
RECOMMENDATION: Name a US Navy Warship-- Destroyer or Frigate--after PO2 Telesforo Trinidad, which follows in the proud tradition of the US Navy in naming a ship after a Medal of Honor Recipient.
POINT OF CONTACT: Cecilia I. Gaerlan
Email: cecilia@bataanlegacy.org; Cell: (510) 520-8540